What you carry may contribute to your back pain and neck pain: Backpack vs Shoulder bag
With the start of the fall season, most of us are packing away our suitcases and picking up our backpacks and shoulder bags to return to school and work. Could your bag choice be contributing to your back pain? Is there a bag type better suited for carrying items daily? While traveling with a bag, it’s important to be considerate about how the bag affects posture and therefore contributes to back pain you are experiencing. Let’s compare two of the most typical bag types, shoulder bags and backpacks.
When carrying a shoulder bag, we must be mindful of the distribution of weight on either side of our shoulders and back. When we carry a shoulder bag on one side for too long, we may, after a while, favor the side that we are carrying the bag on. This can change our normal gait and cause stress on the muscles on the opposite side. Another aspect to consider of shoulder bags is the weight you are carrying. When carrying a heavy shoulder bag, we can subconsciously lean to the opposite side to compensate for the unequal weight distribution.
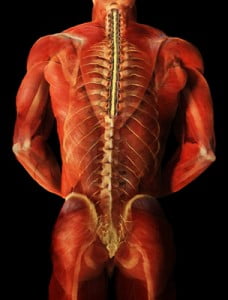
Studies show that carrying a back pack often lessens back pain one may experience compared to a shoulder or cross-body bag. With straps on both shoulders, there is better weight distribution and less strain on one side of the back or neck. A study at a university determined that students carrying materials in one-shoulder bags had significantly greater activity in the trapezius muscles than their peers who carried back packs. Greater activation in the shoulder muscles is likely due to the constant contraction of the shoulder muscles while carrying bags that are heavy or to one side. Constant contraction of the muscle or spasm can be very painful and if not treated or released can lead to hypersensitivity of the nerves that sense pain. Over time you may find that even smaller amounts of weight can cause pain in your back and spread to other areas. While carrying a backpack, choose a bag that has wide straps and cushion for additional comfort. Small straps, although on both shoulders, may still cause discomfort because the weight of the bag is concentrated in a smaller area.
Lastly, after selecting the kind of bag you would like to carry, consider how much weight you are carrying in your bag. Studies have shown that carrying greater than 10% of your body weight can be detrimental to your back and neck health. Try carrying as few things as possible when traveling and consider other methods to access things you may need. For example, use electronic storage for documents or books to avoid carrying excessive weight. In addition, choose lighter materials and avoid heavier materials if possible.
To summarize, here are things you can do to reduce back pain when carrying a bag:
– If you can, go for a back pack instead of a shoulder bag,
– Choose a bag with wide straps for even weight distribution.
– Try to carry the least amount of weight you can if possible.
If you are experiencing chronic back pain, call the Norman Marcus Pain Institute where we can assess your pain for potential treatment options.
References
Hardie R, Haskew R, Harris J, Hughes G. The effects of bag style on muscle activity of the trapezius, erector spinae and latissimus dorsi during walking in female university students. J Hum Kinet. 2015 Apr 7;45:39-47. doi: 10.1515/hukin-2015-0005. PMID: 25964808; PMCID: PMC4415842.
Hernández TL, Ferré MC, Martí SG, Salvat IS. Relationship between School Backpacks and Musculoskeletal Pain in Children 8 to 10 Years of Age: An Observational, Cross-Sectional and Analytical Study. Int J Environ Res Public Health. 2020 Apr 5;17(7):2487. doi: 10.3390/ijerph17072487. PMID: 32260533; PMCID: PMC7177975.







 grabbing more grand slam titles, if Nadal’s stem cell treatment is being used to eliminate his pain by repairing his joints or discs, the actual cause of his back pain may not be addressed.
grabbing more grand slam titles, if Nadal’s stem cell treatment is being used to eliminate his pain by repairing his joints or discs, the actual cause of his back pain may not be addressed.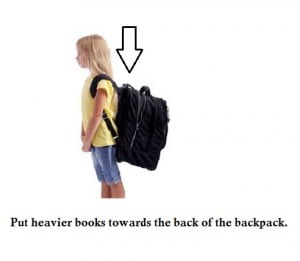

 As I mentioned in an earlier blog, “
As I mentioned in an earlier blog, “