Men:
Where do you keep your wallet? Many of you probably answered, “your back pocket.” Did you know that this could be causing your back pain?
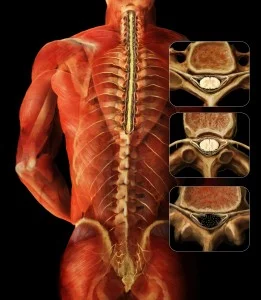
When you sit down with your wallet in your back pocket, it presses into your muscles, which can cause pain in your low back and buttock. The squeezed muscle can press your sciatic nerve causing the pain to travel down your leg.
If you’re suffering from back pain, try keeping your wallet in an external bag or a front pocket. Or simply decrease the thickness of your wallet by taking out any extraneous items, such as old receipts or credit cards that you no longer need or use.
Women:
Those fashionable Jimmy Choos or Manolo Blahnik’s, which are known for their height, may actually be increasing your low back pain. But don’t switch out those high heels for the increasingly popular ballet flats or stylish sandals because flats can stretch and strain the muscles in the calves and thighs causing pain in the buttock and low back.
You don’t have to forgo fashion for comfort. Wearing low, comfortable heels can save your back from unnecessary pain. Remember to wear shoes that fit properly as well – ill-fitting shoes can cause you to tighten your leg and buttock muscles causing low back, buttock, and leg pain.
Children:
Now that school is back in session, many kids are carrying heavy books in their backpacks. Often, the heavy, incorrectly worn backpacks can cause poor posture and strain on muscles. Parents, have your child(ren) pack their backpacks so that the heaviest books are placed towards the back of the bag. This way, the heaviest part of the bag is closer to the back of the child. (see picture) Also, remind your child(ren) to use both straps on both shoulders. This helps distribute the weight evenly, as opposed to placing strain on one shoulder. Another option is using backpacks with rolling capabilities.
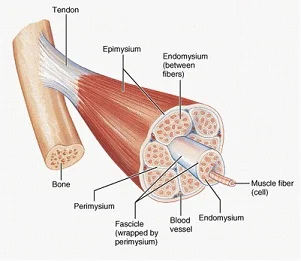
Similarly, all you ladies who stuff your shoulder bags with everything from lipstick to workout weights, carrying a heavy bag on your shoulder every day can be the source of your aching neck and back. While those oversize totes conveniently contain everything you might possibly need in a day, the accumulated stress on your neck and spine from “pocketbook overload” can lead to serious strain on your muscles, tendons, nerves, and ligaments, causing serious body aches. So what does a fashionable woman on the go do?
- If you absolutely must carry a tote, lighten the load – try to take out the items you don’t really use or need.
- Switch the bag from one shoulder to the other often, minimizing the amount of time you strain the shoulder and neck muscles.
- Try using two lighter bags instead of one big one. Splitting the load and carrying them on both sides distributes the weight evenly.
And don’t forget; no matter what you carry, having good posture helps reduce back pain.
Parents:
Lifting your baby 50 times per day, or bending and lifting up to get your active toddler out of his/her sibling’s hair, are innocent movements that can indeed cause low back pain. Good posture and proper lifting techniques can help parents avoid the increased risk for low back pain. Some key pointers:
- Keep your feet (shoulder width) apart, your back straight and bend your knees to reach for your child.
- Use your leg muscles, which are bigger and stronger than your back muscles, to lift your child. After you bend over, bring your child to your chest, bring your back to the upright position, and then straighten your legs. If you straighten your legs before bringing your body upright, you’re using your low back muscles to lift your child. However, if you straighten your legs last, then you’re using your leg muscles.
Keep in mind; this is a good tip for lifting anything heavy!



 I found a few patients who had not been honest with me and had received medications from other doctors. Unfortunately, the small occurrence of dishonest behavior has obliged all doctors to be alert for the possible misuse of medication. At the
I found a few patients who had not been honest with me and had received medications from other doctors. Unfortunately, the small occurrence of dishonest behavior has obliged all doctors to be alert for the possible misuse of medication. At the  Some opioids, such as oxycodone, are often combined with Tylenol (
Some opioids, such as oxycodone, are often combined with Tylenol (