Dr. Marcus learned about the importance of muscles from his mentor, Dr. Hans Kraus. Dr. Kraus taught Dr. Marcus how to examine the body for muscle pain and how he treats each muscle. Dr. Kraus was known as one of the fathers of sports medicine. He is also known for having treated President John F Kennedy’s back pain.
back pain posts Archives
Dr. Hans Kraus – Mentor to Dr. Marcus
How important is your diagnosis?
 I met a lovely 53 year old gentleman, who was suffering from severe low back and hip pain for over a year, diagnosed with a herniated disc. He had tried physical therapy with some relief, but still was unable to eliminate his pain. After diagnosing and treating muscles in his low back, buttock, and thigh, he reported no low back pain, and was discharged from our office. However, after five years, he returned to our office, stating that he had foot pain, diagnosed with plantar fasciitis, and unable to rock climb or hike without severe pain in his calves and feet. After identifying and treating multiple muscles in his calves, shins, and feet, he reported 100% relief, and even finished a 10 day rock climbing trip. Although you may be given one diagnosis, sometimes we find muscle involvement and are able to eliminate the pain!
I met a lovely 53 year old gentleman, who was suffering from severe low back and hip pain for over a year, diagnosed with a herniated disc. He had tried physical therapy with some relief, but still was unable to eliminate his pain. After diagnosing and treating muscles in his low back, buttock, and thigh, he reported no low back pain, and was discharged from our office. However, after five years, he returned to our office, stating that he had foot pain, diagnosed with plantar fasciitis, and unable to rock climb or hike without severe pain in his calves and feet. After identifying and treating multiple muscles in his calves, shins, and feet, he reported 100% relief, and even finished a 10 day rock climbing trip. Although you may be given one diagnosis, sometimes we find muscle involvement and are able to eliminate the pain!
Insurance Blog 101
When you hear the word insurance, I’m sure we all groan a little (or maybe a lot). A big part of this frustration is not knowing. We don’t understand the rules (which constantly change), we don’t  understand the jargon, and we don’t have a roadmap to navigate this nightmare. I’m not going to lie – it is not a simple and easy system, and I don’t have the answers to all the problems. However, my goal is always to teach what I know, to help someone create a roadmap, understand the jargon and perhaps get through some of the problems they may be experiencing. If you have questions that you would like to send, I will do my best to answer all of them.
understand the jargon, and we don’t have a roadmap to navigate this nightmare. I’m not going to lie – it is not a simple and easy system, and I don’t have the answers to all the problems. However, my goal is always to teach what I know, to help someone create a roadmap, understand the jargon and perhaps get through some of the problems they may be experiencing. If you have questions that you would like to send, I will do my best to answer all of them.
Patient Story – Meet Parker
I had the pleasure of meeting Parker (name changed for privacy) a few years ago. I met Parker after he had extensive surgery related to his progressive scoliosis. He reported pain in his chest, spine, and neck. He had received many nerve block injections to his spine without relief. His physical examination identified multiple muscles as a source of his pain.
After treatment to various muscles in his upper and lower body, Parker reported significant relief in pain. He was able to start playing ice hockey and running in 10K races.
Although Parker had a successful fusion to treat his curving spine, he still had severe pain, which came from altered muscle tissue. Muscle treatment plus the fusion allowed Parker to reclaim his life. Without the addition of muscle treatment, a successful surgery would not have had a good outcome.
NMES versus TENS
What is the difference between NMES and TENS?
Simply put, NMES, or neuromuscular electrical stimulation, also known as EMS (electrical muscle stimulator), causes muscle contractions, and TENS produces a sensation to compete with the pain sensation. NMES is provided by a device that attaches to electrodes, which are placed onto your skin over a muscle you want to stimulate. Muscle stimulation causes the muscle to contract the way it would if you were exercising the muscle, so NMES can help with a muscle that has gotten smaller (atrophy) or suffers from spasms or swelling (edema). TENS is a handheld instrument that sends an electrical impulse to the nerves in the skin on the painful area. When it does its job, you feel a buzzing sensation instead of your usual pain.
Patient Story – Meet Joe
I met Joe, a 43 year old male, who suffered from bilateral (both) shoulder pain for 2 years. He had tried trigger point injections, botox injections, radiofrequency ablations (burning of the nerves), and even surgery, all without relief.
I started Joe’s treatments with photobiomodulation (also known as low level laser therapy) with resultant 50% relief in pain. Then, I treated specific muscles I identified as a source of pain – Serratus Anterior, Subscapularis, Latissimus Dorsi, and Levator Scapula – with muscle-tendon injections followed by three days of physical therapy.
I followed Joe for six months following the end of the treatment. Joe’s pain went from an 8/10 to a 1/10, and he reported no interference in his activities of daily living. He was even able to resume running, and stopped all pain medications without any return of his pain.
A common link between pain and allergies
Do you have widespread pain? Do you also have allergy symptoms like itching, hives, or wheezing? Did you know that allergy symptoms and bodily pain are both symptoms of a common condition?
If any of these questions resonate with you, you could have Mast Cell Activation Syndrome (MCAS), a condition that causes both pain and allergy symptoms. MCAS is a common condition that may impact up to 17% of the population.
If you have never heard of MCAS, that’s because MCAS is a condition that is only gaining widespread recognition in the past decade or so through a recent boom in research. There are many doctors who are not familiar with MCAS, but as research grows on the condition, doctors are becoming aware of how and when to diagnose it.
If you have allergies and pain symptoms, you may have never thought about how these two seemingly unrelated symptoms might be a sign of a single condition. If you have MCAS, or think you might, we encourage you to learn more about a clinical trial opportunity we are holding at our clinic.
Why Mast Cell Activation Syndrome is a tricky diagnosis
Mast Cell Activation Syndrome (MCAS) is a common condition that can cause widespread pain in the body as well as allergy symptoms like hives, itchy skin, and congestion. MCAS is hard for doctors to diagnose for a few reasons. The main reason is that it is an under researched condition despite its commonality. Doctors are only recently starting to understand just how common MCAS is, and how important it is to study it.
MCAS has a lot of symptoms that aren’t frequently associated with each other. In fact, MCAS symptoms can occur all over the body, for example, the skin (hives), the gastrointestinal system (stomach pain), the cardiovascular system, or the respiratory system. With these seemingly unrelated symptoms, MCAS presents as a confusing condition to those who are unfamiliar with it. It is a condition that may even require multiple experts to treat due to its vast range of symptoms.
Thankfully, more and more primary care providers are learning about this common condition that may affect up to 17% of the general population, as research has been expanding greatly in the past decade. More treatment options are currently being developed in the clinical trials stage. If you have MCAS, or think you might, we encourage you to learn more about a clinical trial opportunity we currently have in our clinic.
Sitting with your legs crossed may be contributing to your back pain
Think of some of the ways you sit. Whether taking a ride on the subway, waiting patiently at the doctor’s office, or sitting as a passenger in a car, the way we sit, especially for prolonged periods can have an effect on the pain we may experience in our low back.
For many of us, sitting with our legs crossed feels comfortable in the moment but have you ever considered how this can affect your back and cause pain? What happens to your spine and muscles when sitting with your legs crossed for an extended period of time? When considering good posture, a large component is keeping your spine neutral and avoiding positions that twist the spine or cause misalignment. When sitting with your legs crossed, your pelvis becomes tilted and unconsciously, we tilt our entire torso towards one side. There is a curvature towards one side in the low back which then creates problems in other areas of the spine. Naturally, with a tilt of the pelvis, the upper body will compensate by leaning the opposite direction to maintain balance. Working from the bottom up, pressure on the lumbar spine will cause curvature and misalignment in the thoracic spine. This places strain on the cervical spine to keep the head in the upright position.
Sitting with our legs crossed can also affect our muscles. There are two common sitting positions that we should be mindful of, knee over knee or foot over knee for a prolonged period can cause a tightness in the hamstrings, hip flexors and glute muscles. The iliopsoas, one of the major hip flexor muscles, is responsible for external rotation of the femur and an integral part in maintaining posture. This muscle may become strained due to contraction while the pelvis is tilted. You may notice soreness and tenderness in the low back and hip area. Similarly, sitting foot over knee can over time damage the muscles in the inner thigh. Most commonly, the sartorius muscle can become tight and cause discomfort when sitting with the calf over the knee. At the Norman Marcus Pain Institute, Iliacus and Psoas muscles on the hip can be treated for pain. As one of the most common muscles causing pain for patients, when treated, the Iliacus and other hip flexors can provide great relief for pain in the low back, buttock and groin.
Instead of sitting with crossed legs, sit in a chair with height necessary to place both feet flat on the floor. While sitting upright with your back against the chair, you may want to consider placing a cushion under your bottom that can add support to the low back.
References
Lee BJ, Cha HG, Lee WH. The effects of sitting with the right leg crossed on the trunk length and pelvic torsion of healthy individuals. J Phys Ther Sci. 2016 Nov;28(11):3162-3164. doi: 10.1589/jpts.28.3162. Epub 2016 Nov 29. PMID: 27942141; PMCID: PMC5140821.
Best Posture for Reading: How to alleviate back pain
There’s nothing better than snuggling into a good book. But are you experiencing back pain while sitting and reading for an extended period? Back pain can often be caused by improper posture. While reading, whether using a physical book or an electronic device, many people experience back pain in the neck and shoulder or in the low back. Here are some ways to alleviate back pain while reading.
Reading can cause strain on the neck and shoulders if there is a tilt in the neck to look down at your book or device. While sitting and reading, it’s important to place your reading material at eye level. Sitting with your head leaning forward and back hunched can cause hyperflexion of the cervical spine and lead to severe neck and back pain over time. It is best to use a stand that can be adjusted to the required height. Many have recommended raising your materials with your hand; however, this may also cause some strain on the neck and shoulders. While holding an object in front of you at eye level, either with one or both hands, your shoulder and neck muscles are in constant contraction to sustain this positioning. Even over a period of a few minutes, this can cause the muscles to spasm or cause intense strain. Using an adjustable stand will ensure that we can sit straight up, taking pressure off of the cervical spine.
The best posture for reading is sitting upright in a chair with lumbar support. Avoid sitting on a seat that lacks back support such as a stool or a bench. A chair with good ergonomics is one that supports the low back and provides an arm rest to place both elbows. Mentioned above, we want to avoid stiffness in the upper back and neck muscles. Placing your elbows on an arm rest that is low enough to support your arms without adding additional strain is ideal. A study examining the association of low back pain with cell phone use found that thoracolumbar kyphosis and lumbar lordosis (curvature in the spine causing a pelvis tilt) increased with prolonged sitting. Participants had a slouch and progressed spine curvature after sitting for longer than 30 mins. The study also found that those with pre-existing back pain had a significantly higher increase in lordosis and complained of more back pain. When sitting for longer than 30 minutes, take breaks. Sitting should be interrupted by standing breaks to keep blood flowing and reduce stiffness in muscles.
To summarize, here are some things we can do to minimize back pain while reading or using a device while sitting.
– Sit with back and arm support for your neck and shoulders
– Bring your reading material or device to eye level to avoid neck strain
– Take breaks and stand for a minute or so while sitting for more than 30 minutes
References
In TS, Jung JH, Jung KS, Cho HY. Spinal and Pelvic Alignment of Sitting Posture Associated with Smartphone Use in Adolescents with Low Back Pain. Int J Environ Res Public Health. 2021 Aug 7;18(16):8369. doi: 10.3390/ijerph18168369. PMID: 34444119; PMCID: PMC8391723.
How your sleeping position affects your back pain and neck pain
We all have different preferences when it comes to sleeping. Some of us are side sleepers while others may prefer to sleep on our backs. But there may be a few things to consider about your sleeping position that may be contributing to your back pain. Here are three ways to sleep to help prevent back pain and get a good night’s rest.
Sleeping on your side.
When laying on your side. Be sure to first support your head and neck. This can be done by placing as many pillows or supports as needed to keep the cervical spine neutral and the muscles surrounding it relaxed. These pillows or supports should be placed in the gap between the neck and the head, until the head is upright. Try to avoid raising your arm above your head as this may cause additional strain in the neck and shoulders. To keep the lumbar spine as neutral as possible, place a pillow between your knees. You may need to find a pillow that has enough support to hold the leg. This prevents the hips from rotating forward toward whichever side you are leaning on and helps to prevent rotation in the hips.
Sleeping on your back.
The recommendations for sleeping will be the same with slight adjustments for positioning. You must support your head and neck while sleeping on your back. This can be accomplished by placing your pillows in the gap between your neck and the bed while ensuring the top of the head is also lifted. This prevents an over extension of the cervical spine. Secondly, place a pillow under your knees to raise them slightly above the pelvis. This tilts the sacrum and the spine to neutral position.
Sleeping on your stomach/front.
A study on the relationship between sleep posture and spinal symptoms found that the prone sleeping position or sleeping on your front is the largest contributor back pain and poor quality of sleep. Although this sleeping position is not recommended for extended periods of time. If you need to sleep on your front, place a pillow under your hips to prevent curvature in the lower back. Additionally, a pillow should be placed under the ankles to provide comfort for the knees and avoid hyper extension of the hamstrings. Although it may be comfortable in the moment, raising a knee to either side may cause additional rotation in the sacrum and over time cause strain on the hip flexor muscles and muscles surrounding the spine.
To summarize, here are some ways you can avoid back pain while sleeping:
– Support your head and neck
– Avoid curvature in the back and rotation of sacrum for an extended period of time.
– Use pillows when necessary for additional comfort.
References
Cary D, Briffa K, McKenna L. Identifying relationships between sleep posture and non-specific spinal symptoms in adults: A scoping review. BMJ Open. 2019 Jun 28;9(6):e027633. doi: 10.1136/bmjopen-2018-027633. PMID: 31256029; PMCID: PMC6609073.
Cary D, Jacques A, Briffa K. Examining relationships between sleep posture, waking spinal symptoms and quality of sleep: A cross sectional study. PLoS One. 2021 Nov 30;16(11):e0260582. doi: 10.1371/journal.pone.0260582. PMID: 34847195; PMCID: PMC8631621.
Back Pain and Neck Pain – how your bag may affect it
What you carry may contribute to your back pain and neck pain: Backpack vs Shoulder bag
With the start of the fall season, most of us are packing away our suitcases and picking up our backpacks and shoulder bags to return to school and work. Could your bag choice be contributing to your back pain? Is there a bag type better suited for carrying items daily? While traveling with a bag, it’s important to be considerate about how the bag affects posture and therefore contributes to back pain you are experiencing. Let’s compare two of the most typical bag types, shoulder bags and backpacks.
When carrying a shoulder bag, we must be mindful of the distribution of weight on either side of our shoulders and back. When we carry a shoulder bag on one side for too long, we may, after a while, favor the side that we are carrying the bag on. This can change our normal gait and cause stress on the muscles on the opposite side. Another aspect to consider of shoulder bags is the weight you are carrying. When carrying a heavy shoulder bag, we can subconsciously lean to the opposite side to compensate for the unequal weight distribution.
Studies show that carrying a back pack often lessens back pain one may experience compared to a shoulder or cross-body bag. With straps on both shoulders, there is better weight distribution and less strain on one side of the back or neck. A study at a university determined that students carrying materials in one-shoulder bags had significantly greater activity in the trapezius muscles than their peers who carried back packs. Greater activation in the shoulder muscles is likely due to the constant contraction of the shoulder muscles while carrying bags that are heavy or to one side. Constant contraction of the muscle or spasm can be very painful and if not treated or released can lead to hypersensitivity of the nerves that sense pain. Over time you may find that even smaller amounts of weight can cause pain in your back and spread to other areas. While carrying a backpack, choose a bag that has wide straps and cushion for additional comfort. Small straps, although on both shoulders, may still cause discomfort because the weight of the bag is concentrated in a smaller area.
Lastly, after selecting the kind of bag you would like to carry, consider how much weight you are carrying in your bag. Studies have shown that carrying greater than 10% of your body weight can be detrimental to your back and neck health. Try carrying as few things as possible when traveling and consider other methods to access things you may need. For example, use electronic storage for documents or books to avoid carrying excessive weight. In addition, choose lighter materials and avoid heavier materials if possible.
To summarize, here are things you can do to reduce back pain when carrying a bag:
– If you can, go for a back pack instead of a shoulder bag,
– Choose a bag with wide straps for even weight distribution.
– Try to carry the least amount of weight you can if possible.
If you are experiencing chronic back pain, call the Norman Marcus Pain Institute where we can assess your pain for potential treatment options.
References
Hardie R, Haskew R, Harris J, Hughes G. The effects of bag style on muscle activity of the trapezius, erector spinae and latissimus dorsi during walking in female university students. J Hum Kinet. 2015 Apr 7;45:39-47. doi: 10.1515/hukin-2015-0005. PMID: 25964808; PMCID: PMC4415842.
Hernández TL, Ferré MC, Martí SG, Salvat IS. Relationship between School Backpacks and Musculoskeletal Pain in Children 8 to 10 Years of Age: An Observational, Cross-Sectional and Analytical Study. Int J Environ Res Public Health. 2020 Apr 5;17(7):2487. doi: 10.3390/ijerph17072487. PMID: 32260533; PMCID: PMC7177975.
The Start of Baseball Season
The baseball season just opened and already players are calling off their first few games due to “tweaked knees” and “sore backs”. As the sun is starting to come out, and the snow is (FINALLY!) melting, many of us are anxious to get outside and start playing sports again. However, this is also a time where pain can start rearing its ugly head. Many people forget to limber and stretch properly before AND after playing sports, causing strains and sprains of muscles.
So keep in mind these important tips to get moving again this spring:
- Do gentle limbering stretches every day to help maintain flexibility of your muscles.
- Stretch before and after any exercise.
- Start slowly – if you haven’t moved all winter, start with simple exercises, like walking, before starting anything more difficult.
- If you’re feeling extremely sore the following day, it means you may have done too much. Cut back on the difficulty and amount of time the next time you exercise. Slowly increase the difficulty and the length of the session. A safe rule of thumb is to start out after a long layoff at 50% of your prior routine and then increase 15-20% every 5-7 days as long as you feel okay at any level before going to the next.
- Drink lots of water!
Acetaminophen
The BMJ (what used to be called the British Medical Journal) just published an article stating that acetaminophen (ie Tylenol) has been found to provide no relief in low back pain (compared to a placebo). Acetaminophen was also related to a risk of having an abnormal liver test. The article included data from 13 randomized controlled trials (RCTs).
An RCT to evaluate a drug is a research study where one group of people receives the actual drug (in this case, acetaminophen) and the other group receives a placebo (a pill with no active ingredient, generally a sugar pill). Then, data is collected from both groups to see if either achieved any pain relief. In this analysis, it shows that whether you receive acetaminophen or a sugar pill, you had the same amount of pain relief – meaning that active drug had no real pain relief effect.
relief. In this analysis, it shows that whether you receive acetaminophen or a sugar pill, you had the same amount of pain relief – meaning that active drug had no real pain relief effect.
Although most of the patients I see find no relief from acetaminophen, a small percentage of patients do, so don’t completely dismiss this drug when it comes to helping your pain. However, if you do take acetaminophen, make sure that you’re not taking too much. The FDA recommends taking less than 3000mg a day. This means if you’re taking Extra Strength Tylenol (500mg), you can only take 6 pills a day, or regular strength, 300mg, 10 pills a day. Higher amounts can lead to liver damage that could even be life-threatening.
Smoking and Back Pain – is it related?
We all know that smoking is bad for you. In fact, since 1965, the Surgeon General’s Warning posted on every package of cigarettes says: Smoking Causes Lung Cancer, Heart Disease, Emphysema, And May Complicate Pregnancy. But did you know that in addition to the myriad of illnesses that are related to tobacco and smoking, recent studies show that smokers have a higher prevalence of back pain than non-smokers? It’s true.
Several studies in the 1980s and 1990s have shown a correlation between smoking and increased back pain. More recently, a  meta-analysis was done in 2010, which basically means a large number of studies (in this case, 40) were put together, and the results were compared to see what pattern, if any, existed between back pain and smoking. This meta-analysis concluded that current and former smokers have a higher prevalence of back pain. It even made the comparison between adult smokers to adolescent smokers; adolescents showed a higher prevalence of back pain. Therefore, we can conclude, the earlier one smokes, the greater risk to your back.
meta-analysis was done in 2010, which basically means a large number of studies (in this case, 40) were put together, and the results were compared to see what pattern, if any, existed between back pain and smoking. This meta-analysis concluded that current and former smokers have a higher prevalence of back pain. It even made the comparison between adult smokers to adolescent smokers; adolescents showed a higher prevalence of back pain. Therefore, we can conclude, the earlier one smokes, the greater risk to your back.
Is there a technical or medical reason behind this connection? Indeed. Smoking causes constriction of blood vessels, which reduces the amount of blood going to your muscles. Decreased blood results in decreased oxygen, which is one of the most important factors in initiating muscle pain. Some smokers actually had parts of their arms and legs amputated because of dead tissue caused by too little oxygen.
Do you want be free of back pain? Put out that cigarette and quit smoking!
When Making Medical Decisions About Pain Relief, Is More Information Better?
In today’s world we are bombarded by information and ways to obtain it. Do you want to know how many steps you take a day? Just buy a device and it will calculate it for you. Care to know what your cholesterol levels are? Simply go get a kit at your nearest drug store. Is it possible we are gathering too much information for our own good?
The same question can be asked about medical testing. Is it useful or even helpful to know certain things about our bodies? Many of us have undoubtedly had the experience where we have gone to the doctor because we had pain and an imaging study was ordered. MRI, CT, and ultrasound can give us information about our bodies that would have been unimaginable in the past.
While technology in general is of course a huge benefit, at the Norman Marcus Pain Institute, we believe it is necessary to proceed with caution as we navigate through it all. At NMPI, one common problem we find in back pain, neck pain, and shoulder pain is the overuse and overreliance on imaging studies. “Abnormalities” are often found on imaging studies without any relation to one’s pain. In fact, seeing abnormalities is more common than seeing a “normal” spine! For example, up to 40% of people without back pain can have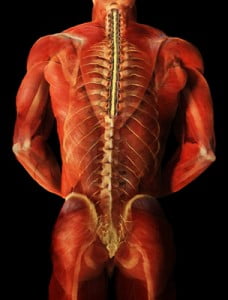 herniated discs and as many as 70% may have degenerated discs. That is why the US Institute of Medicine suggests not getting an MRI too quickly since you are likely to see one of these problems and assume it is the cause of your pain. This can lead to unnecessary nerve blocks and surgery.
herniated discs and as many as 70% may have degenerated discs. That is why the US Institute of Medicine suggests not getting an MRI too quickly since you are likely to see one of these problems and assume it is the cause of your pain. This can lead to unnecessary nerve blocks and surgery.
At NMPI, we often see patients who have a herniated disc, yet they only have pain in their back and buttock. They have not experienced any radiation into the leg(s) at all. In these patients, the pain generally has nothing to do with the disc herniation since disc herniation pain generally radiates down the leg and into the foot. Even when the patient is experiencing pain down the leg with a herniated disc found on MRI, muscles in the low back and buttocks may be the cause of the pain. If muscles are not examined as a potential cause, you may undergo an apparently reasonable surgery, without achieving relief of pain. Some studies show that up to 50% of spine surgeries fail (resulting in failed back surgery syndrome) and one of the reasons is the failure to identify muscles that were the true source of the pain.
Most back pain and neck pain is caused by soft tissue such as muscles and tendons. This is confusing because you may have been told your pain is from your spine, discs, or nerves. The problem is most people as they get older have signs of wear and tear on their x-rays and MRIs, but these common signs of aging may not explain your pain if the pain actually originates in your muscles. That’s why we say, when diagnosing persistent pain it’s not having “more” information at hand, it’s having the “right” information at hand.
At NMPI, we often see patients who experience persistent pain even after multiple spine surgeries. Our non-surgical, non-invasive treatment program has most of our patients leaving our office free of long standing back, neck, shoulder, and headache pain.
What To Do When Back Pain Causes Overdose?
“We don’t appreciate what we have until it’s gone.” If only we had a dime for every time we heard this. Perhaps the reason it is such a common expression is the simple truth in it. This certainly applies to our health, but specifically our backs. We probably all take our good health in vain, until something goes wrong. By the time we are in our forties over twenty percent of us experience some form of back pain. And what do we do when we experience pain? Well, unfortunately many people will turn to strong painkillers. This means opioids, morphine-like painkillers. And, while we have written about this topic in the past, there is something new on the horizon. Evzio, the brand name of injectable Naloxone, is a prescription medicine that can block the effects of morphine and related painkillers. Approved by the FDA in April 2014, it allows a patient to quickly treat themselves or be treated by a family member if the patient has overdosed on opioids.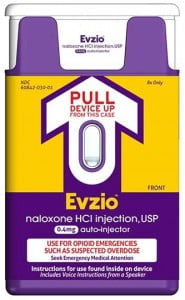
In the past, Evzio was difficult to obtain due to its high cost. However, recently The Clinton Foundation announced that it has negotiated a lower price for Evzio (see NYT article). This will allow municipalities to more easily purchase this medication, making it more available to those who need it.
It is a sad reality that many people will turn, in desperation, to painkillers as an answer to their aching backs. We, at the Norman Marcus Pain Institute, only use opioids as a last resort. Our method of finding the source of the pain and treating it has eliminated back pain for thousands of patients.. Nevertheless, with the rise of overdoses each year, the increased availability of naloxone to non-medical personnel will allow lives to be saved.
Why Health Insurances Carriers Should Not Be For Profit Enterprises
In November, I read this article in The New York Times on How Medical Care Is Being Corrupted. In a nutshell — Insurance carriers have been incentivizing care for more than 20 years by selectively paying for some services whilst denying others.
To successfully address a complicated problem, such as long-standing pain, more than one approach is often most effective albeit initially more expensive. As a Pain Medicine physician, I have witnessed the defunding of the only approach that has been found to be consistently successful (by the Cochrane database for systematic reviews) in addressing patients disabled by chronic back pain: comprehensive multidisciplinary pain treatment centers.
While cost should be a consideration in choosing treatment – it should not be the primary deciding factor. For-profit insurance companies can be effective in helping policyholders fund their medical care but they are constrained by conflicting interests
- A moral and ethical obligation to care for policyholders who have purchased a policy to protect their health.
- Shareholders who have invested in the company and expect each quarter to produce a reasonable profit.
If you believe, as I do, that health insurance not be allowed to be a for profit enterprise, join in a national discussion to legislate that all health insurance be not-for-profit. Insurance companies should only exist for the protection of the individual patient.
Rafael Nadal will receive stem cell therapy for back pain – Should You?
Earlier in November, Rafael Nadal, the 14-time Grand Slam winner, announced he would receive stem cell treatment to help heal his ailing back, the same type of treatment he received for his knee. His doctor in Barcelona, Dr. Angel Ruiz-Cotorro, who has been treating Nadal for 14 years, said, “Nadal’s back pain is ‘typical of tennis’ players in that the treatment is meant to help repair his cartilage.” Stem cells were recently extracted from Nadal for a cultivation process to “produce the necessary quantities,” said Ruiz-Cotorro. Once cultivated, the stem cells will be placed into the joints of his spine with the goal of regeneration of cartilage as well as for an anti-inflammatory effect. Dr. Ruiz-Cotorro predicts that Nadal can return to training in early December.
Will stem cell treatment work for Nadal’s Back Pain?
Stem cell treatment may seem logical in certain situations – for example, if you have a mechanical problem where a knee has worn out cartilage, causing bone to rub against bone, it makes sense to use stem cells to grow new cartilage to have a cushion to protect the bone and cause the knee to be less painful. As much as we may want to see him back on the courts  grabbing more grand slam titles, if Nadal’s stem cell treatment is being used to eliminate his pain by repairing his joints or discs, the actual cause of his back pain may not be addressed.
grabbing more grand slam titles, if Nadal’s stem cell treatment is being used to eliminate his pain by repairing his joints or discs, the actual cause of his back pain may not be addressed.
Where does back pain originate?
The number one reason for back pain is muscular and other soft tissue, yet muscles are rarely evaluated as the cause of back pain. The only way to determine if Nadal’s back pain is from soft tissue and similar to most people with back pain would be a physical examination of Nadal’s back that included identifying possible muscles as the cause of his pain.
Some doctors believe that the disc, the cushion between the bones of the spine (the vertebra), is a major cause of back pain. They believe that surgeries to correct the flattening or herniation of the disc will decrease or eliminate back pain. Sometimes they are right, but they are just as likely to be wrong. The truth is that there is as high as a 50% failure rate for spine surgeries that were done to eliminate back pain thought to be related to disc problems. There are other joints in the spine that are thought to cause pain; one of them is the facet joint, which could also be a target for stem cell treatments.
When doctors rely on an MRI or CT scan to determine the source of the pain, the information obtained is often confusing. If a surgeon sees an abnormality on an MRI, he will often point to that abnormality as the cause of the pain; in my experience the abnormality found on an MRI or CT scan frequently is not the cause. In fact, if you randomly selected 100 people off the street, and perform an imaging scan, 40 may present with a herniated disc and have no pain and absolutely no awareness of their herniated disc; 70 may have degenerated (worn) discs with no pain, and a large number will have facet joint abnormalities. Therefore, finding an “abnormality” is more common than not. One, then, can deduce that the abnormality is more likely NOT the source of the pain. So treating the abnormality (with steroid injections, surgery, or stem cells) may therefore not relieve the pain.
Stem Cell Treatment and Sports Stars
Nadal, currently ranked as the number 3 professional tennis player in the world, is not the first sports star to chase after a “miracle cure.” The Denver Bronco quarterback Payton Manning and Yankees pitcher Bartolo Colon both went abroad to seek out stem cell treatment as a quick fix to get back in the game. (They both seem to be doing better overall, but it is inconclusive if the stem cell treatment was the cause of their recovery).
Will it work?
In the laboratory, it has been possible to demonstrate the ability of stem cells (most commonly found in the developing embryo and newborn) to grow new tissue. These cells are like silly putty; they can turn into, or adapt, to become any type of tissue. For example, a stem cell in the right environment in the body could become bone, cartilage or some organ (for example, liver or pancreas). But, it hasn’t been as easy to grow tissue in an actual person. There are some early studies that show that stem cells “may” relieve back pain, but both the doctors who are testing the technique and outside experts say much more research is needed before they can say whether the treatment offers real relief.
The use of stem cell therapies continues to be a hot topic for debate in the sports medicine and orthopedic surgery worlds. There is no current evidence-based research to prove that it works.
Sir William Osler, a famous physician, once said: “Use every new treatment as quickly as possible before it stops working.” Stem cell treatment needs to be further investigated to determine if stem cell treatments indeed work, and if so, for what conditions?









